Oral Melanoma in Dogs: Causes, Symptoms and Treatment


Written and verified by the biologist Samuel Sanchez
According to estimates, 1 in 4 dogs will get cancer in their lifetime. The probability increases greatly with age, as in their senior stage, up to 50% of dogs may be developing a malignant neoplasm without you realizing it. Oral melanoma in dogs is the most common type of mouth cancer in this species and requires urgent treatment.
The term “melanoma” refers to a number of different swellings, but not all of them occur in the same areas and with the same symptoms. In this article, we’ll review everything an owner should know about the most common mouth cancer in canines.
What is oral melanoma in dogs?
In the first place, it’s necessary to emphasize that the term “cancer” refers to a series of diseases that have something in common: the unbridled growth of a cell line. Due to mutations in DNA, a group of cells begin to grow unlimitedly and much faster than they should, thus creating the dreaded malignant tumor.
In melanoma, the tumor starts when melanocytes (melanin-producing cells) start to grow out of control. In humans, this condition is always associated with the skin, but we must bear in mind that dogs have pigmentation inside the mouth. Many dog breeds have dark gums, as well as black spots on the roof of the oral cavity and tongue.
As studies indicate, oral melanoma is the most common type of oral cancer in dogs, representing 14.4% to 45% of the tumors that appear in this region. Some veterinarians go as far as saying that it’s the second most common type of cancer in dogs, regardless of the place analyzed.
The labial mucosa of the jaw is the most vulnerable place, as 53% of oral melanomas grow there.
Causes of melanoma in dogs
Talking about causality in cancer cases is quite difficult, as finding a specific agent that triggers it is very difficult. As we’ve said, the underlying motive is the mutation of the melanocyte cell line, but, beyond that, it’s difficult to infer more.
However, there are some factors that seem to balance the scale towards susceptibility. Among them, we highlight the following:
- Breed: Dog breeds with highly pigmented gums are more prone to this type of cancer. Among them, we can highlight Cocker Spaniels, Poodles, Pekingese, Chow Chow, and Golden Retrievers.
- Age: The majority of canine patients with this type of neoplasm are between 10 and 12 years of age, with a mean of 11.4 years.
- Sex: Males are more predisposed to this melanoma.
Symptoms
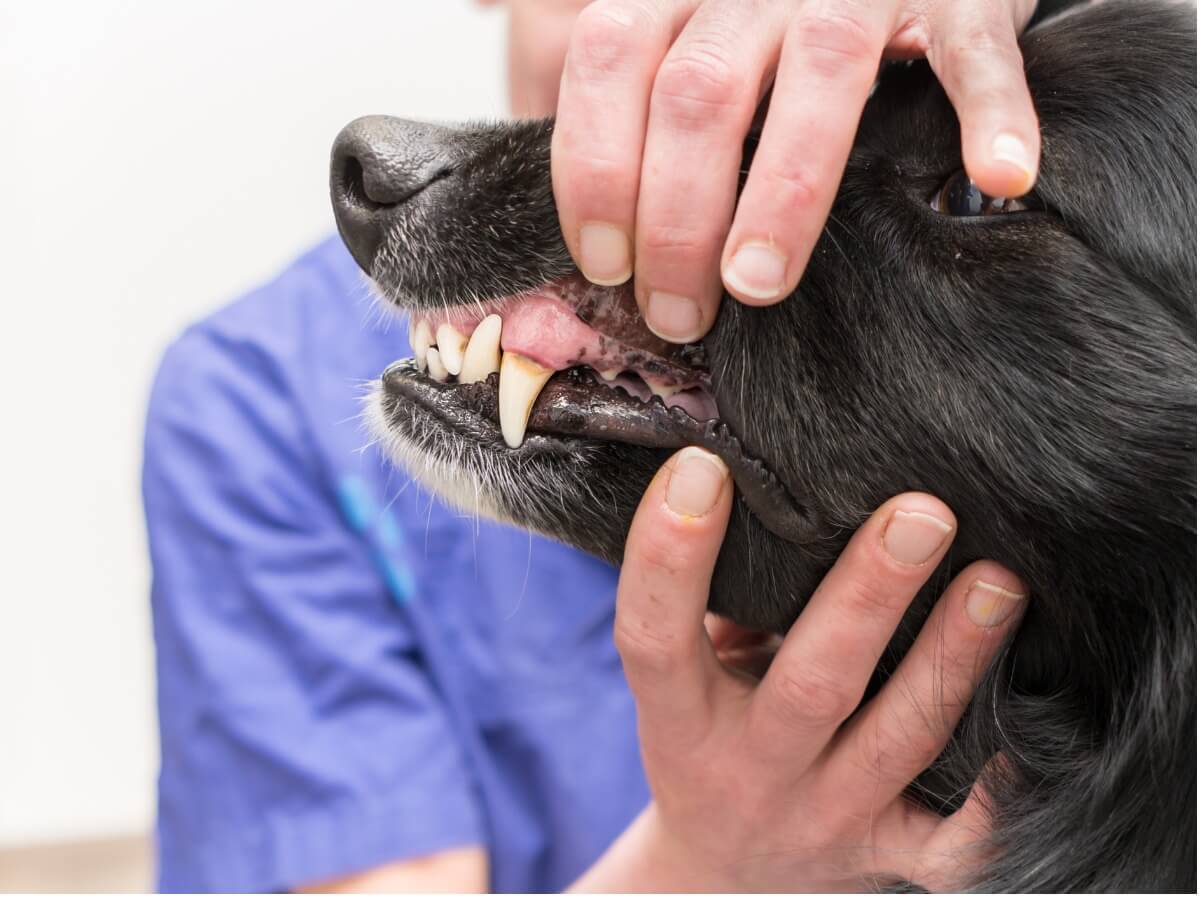
As indicated by the VCA Hospitals veterinary portal, oral tumors appear in the form of hardened pigmented nodules. These can appear anywhere in the mouth and appear small at first, but keep in mind that they tend to extend into the underlying bones and tissues.
Beyond the observable mass, there are other symptoms that can appear, with varying degrees of frequency. Among them, we can highlight the following.
- Increased saliva production (hypersalivation)
- Swelling in one part of the face
- Weight loss
- Foul breath
- Pain
- Inability to eat
- Food falling to the sides of the mouth
- Loss or brittleness in the teeth
In addition, it should be noted that 57% of oral melanomas in dogs spread to the bone, 74% form in the lymph nodes, and cancer cells travel to other organs in 14 to 92% of cases. In the cases in which metastasis occurs, typical symptoms of discomfort will also appear in the newly affected areas.
Diagnosis
The owner who comes to the clinic with the sick dog will almost certainly say that it has difficulty when it comes to eating. In the case of suspected oral cancer, the professional will observe the mass directly and then obtain a sample of the tissue, either by surgical biopsy or cell aspiration. By looking at them under a microscope, they can be confirmed to be cancerous.
Beyond the diagnostic test of the tumor, a complete blood count, a urine analysis and X-rays should be performed on the animal, in order to detect possible metastases in other parts of the body.
The search for metastases in other parts of the body is known as “staging.”
Treatment of oral melanoma in dogs
Surgical resection of the tumor is the indicated treatment in all cases. If the lymph nodes in the neck are affected, they usually have to be removed during surgery as well. However, it’s likely that the nodules will be removed in the same way even if there are no signs of metastasis, as this minimizes the probability that the cancer will spread further.
If the cancer has invaded the bone, part of the dog’s entire jaw may need to be removed. This sounds grotesque, but it will bring a lot of relief to the animal (as it’s a very painful cancer). After surgery, radiation therapy or chemotherapy is also often required to kill any remaining cancer cells.
It’s very possible that the tumor will spread to other areas of the animal’s body, so a systemic approach is usually necessary.

Prognosis and final notes
When it comes to survival rates, it’s necessary to bear in mind that most cancerous tumors in dogs are detected in the last years of their lives. Therefore, the figures aren’t usually very encouraging. In the case of oral melanoma, the survival rate in stage I after surgery is 17-18 months, while in stage III only 3 months of life are reported.
Adding this to the monetary expense, sometimes the best decision is to give the canine palliative treatment and be by their side. The approach will depend on medical opinion, but ultimately the decision whether to attempt aggressive treatment or not is up to the owner.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Bergman, P. J. (2007). Canine oral melanoma. Clinical techniques in small animal practice, 22(2), 55-60.
- Canine oral melanoma, Blue Pearl. Recogido a 25 de agosto en https://bluepearlvet.com/medical-articles-for-pet-owners/canine-oral-melanoma/
- Oral tumors in dogs: melanoma. VCA Hospitals. Recogido a 25 de agosto en https://vcahospitals.com/know-your-pet/oral-tumors-in-dogs-melanoma
- Nishiya, A. T., Massoco, C. O., Felizzola, C. R., Perlmann, E., Batschinski, K., Tedardi, M. V., … & Zaidan Dagli, M. L. (2016). Comparative aspects of canine melanoma. Veterinary sciences, 3(1), 7.
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.