Ringworm in Cats: Causes, Symptoms and Treatments


Written and verified by the veterinarian and zootechnician Sebastian Ramirez Ocampo
Ringworm in cats -also known as dermatophytosis- is a disease in which fungi of various types invade the skin cells, hair, and nails of felines. It’s considered to be the most common fungal infection in cats worldwide. In addition, due to its zoonotic nature, there’s a high risk of transmission from pets to their guardians.
As it’s a major concern for owners, it’s important to know the causes, symptoms, and diagnosis, as well as the best strategies to manage and prevent this important disease in cats. Don’t miss the information below and prepare yourself in the best way in case your feline catches ringworm.
What are the causes of ringworm in cats?
The disease starts with the infection of a cat with fungi called dermatophytes. These microorganisms, having a strong affinity for keratin, attach themselves to the following parts of the host’s body to use them as a source of food and reproduction:
- Skin
- Hair
- Nails
According to an article in the Journal of Feline Medicine and Surgery, the fungus Microsporum canis causes 90% of ringworm in cats, although other types, such as Microsporum gypseum or Trichophyton mentagrophytes, may also be involved.
Transmission can occur by direct contact with an infected feline or with objects contaminated with fungal spores. Among these, the following stand out:
- Nail clippers
- Brushes
- Towels
- Bedding
Although it can occur in cats of any age, breed, or sex, according to the authors of this document, there are certain risk factors for it to occur. Among them, the following can be found:
- Skin lesions: Being the body’s first barrier of defense, a wound in the skin is the ideal entryway for fungi. Attention should be paid to those cats with aggressive play behaviors or that have access to the outdoors. This is because they’re more prone to injury from scratches or bites.
- Immunosuppression: One of the main causes of this condition is prolonged treatment with immunosuppressive drugs such as corticosteroids. Similarly, some studies suggest that cats with diseases such as feline leukemia virus (FLV) and feline immunodeficiency virus (FIV) are more likely to acquire it.
- Ectoparasites: Fleas, in particular, can cause small wounds on the skin. In addition, because of the itching they generate, the cat can hurt itself when scratching.
- Poor hygiene: Inadequate care of the cat can lead to easy colonization by fungi. In addition to this, eradication will be more difficult, as the spores can be spread by the objects used by the pet.
- Overpopulation: In large groups, social stress can predispose cats to suffer from ringworm. In addition, close contact between animals facilitates transmission. Accordingly, stray cats or cats that live in shelters are at high risk of infection.
- Nutritional deficiencies: In particular, diets with low protein and vitamin A levels. These elements play a key role in maintaining a good immune system.
- Young age: Young animals – especially those under one year of age – have an immature immune system. For this reason, their ability to resist infection is more limited. In fact, a study in the Journal of Feline Medicine and Surgery reports that kittens are eight times more likely to suffer ringworm than adults.

What are the symptoms of ringworm infection in cats?
As described above, dermatophytes invade the most keratinous areas of the body, so signs are usually seen in the epidermis, hair follicles, and nails. As stated in an article in The Canadian Veterinary Journal, the following can be distinguished among its symptoms:
- Single or multifocal circular patches with hair loss and desquamation
- Complete areas of alopecia
- Crusty lesions
- Reddening of the skin
- Darkening of the dermis
- Seborrhea
- A strong odor emanating from the cat’s body
- Onychomycosis, which is characterized by weak and brittle nails
- Scratching
As explained in this publication, lesions tend to occur most frequently on the face, ears, and muzzle. However, they can progress to the extremities and other sites, such as the chin.
Can ringworm be transmitted to humans?
The answer to this question is yes. In fact, ringworm is a rapidly spreading pathogen with a high risk of contagion to humans. Moreover, as with pets, young and immunocompromised people are more susceptible to infection by these fungi. This is stated in a paper published in the Journal of Exotic Pet Medicine.
At the same time, a 2022 study reported in the journal Veterinary World reported that people with a history of COVID-19 have a higher risk of suffering from the disease.
Likewise, it’s transmitted through contact with a sick animal or with objects used by the feline. In the event of lesions similar to those described – such as circular patches on the skin – a doctor should be consulted as soon as possible.
How do I know if my cat has ringworm?
Considering that several of these clinical signs are present in other types of skin diseases, the diagnosis should be made by means of laboratory tests. For this, at any sign of disease in your cat, the right thing to do is to see a trained veterinarian immediately.
A paper from the journal Veterinary Dermatology states that different techniques are used to identify the fungus that causes ringworm in cats. The following is a review of some of them.
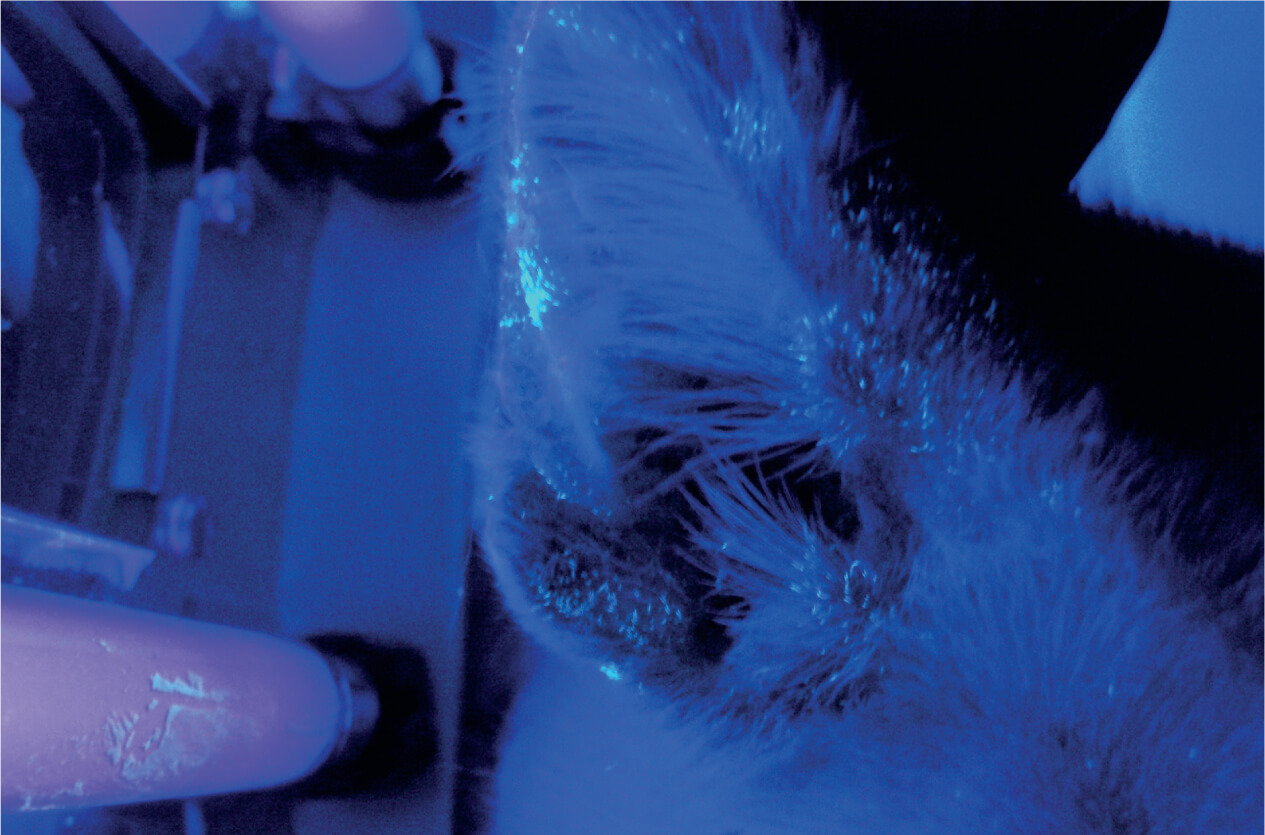
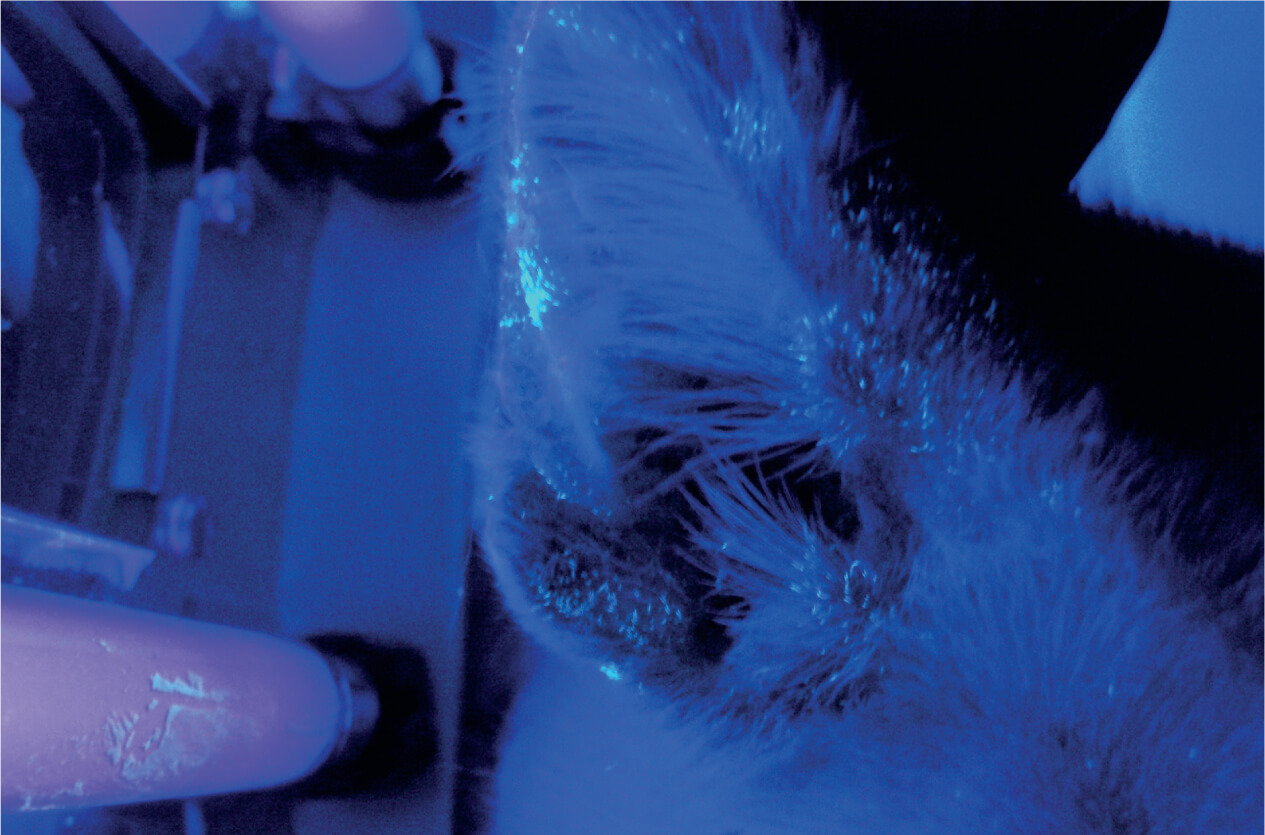
Wood’s lamp
This is an object that emits and receives ultraviolet light wave radiation. Its efficiency lies in the fact that in the case of dermatophyte infections, such as Microsporum canis, the lamp produces a green luminescence as a result of the chemical interaction of the fungus with a metabolite present in the hair.
Therefore, by bringing it close to the cat’s body at a distance of 1 to 2 inches, the hair follicles acquire a glowy hue.
However, it’s important to note that the absence of this fluorescence doesn’t rule out dermatophyte infection, so other tests must be performed to confirm the diagnosis.
Dermatoscopy and trichography
This consists of observing the condition of the skin and coat of the affected animal in an amplified manner. Thanks to this technique, changes such as darkening of the dermis, desquamation, opaque and slightly curved “comma-shaped” hairs, as well as fungal spores can be seen.
Dermatophyte culture
This is a more accurate method of diagnosis. Once the infected skin or hairs are identified, samples are taken by depilation and are isolated in culture media to observe their growth in the laboratory.
It should be noted that false negatives can be obtained if the sample obtained isn’t from infected hairs. The same is true if the storage and incubation conditions are inadequate or if the culture is contaminated with bacteria or other fungi.
How is ringworm in cats treated?
In the event of a positive result for ringworm, the first step to take is to isolate the infected cat. This will prevent the spread of the fungus to other animals, people, or the environment. Then, depending on the severity of the case, the veterinarian may recommend topical or oral therapy or a combination of both.
In the first case, as described in the article Treatment of dermatophytosis in dogs and cats, cream preparations containing miconazole or ketoconazole and shampoos based on miconazole and 2% chlorhexidine are used.
To avoid infecting a person, these medications should be applied with protective gloves.
At the same time, according to this publication, drugs used for oral or systemic therapy include the following:
- Griseofulvin
- Itraconazole
- Terbinafine
These treatments usually last for long periods of at least one to two months. The reason is that dermatophytes are resistant microorganisms, and if medication is stopped early, they may recur.
Among other things, a study published in the journal BMC Veterinary Research reported the effectiveness of a treatment for cats suffering from ringworm that also had leukemia and feline immunodeficiency virus. In this therapy, a “smart microorganism” was used, called Pythium oligandrum.
Finally, all objects used by the feline should be discarded or disinfected. Among them, the following stand out:
- Brushes
- Scratching posts
- Bedding
- Feeders and drinking bowls
How to prevent ringworm in cats?
As you can see, there are several factors that influence the spread of ringworm in cats. Therefore, these tips will help you prevent this unwanted infection in your pet:
- Offer quality and balanced food to your pet: This is in order to keep its immune system in optimal condition.
- Keep strict control over its deworming and vaccination schedule: This way, you’ll be able to avoid diseases, which are the entryway for dermatophytes.
- Avoid letting your cat outdoors: Being outdoors puts your pet in contact with stray cats that could be contaminated.
- Take adopted cats to a veterinarian: It’s also important to avoid contact with other cats for at least three days.
- Take precautionary measures (use of gloves and isolation): If your cat acquires the fungus, these measures will help prevent contagion.
Pay attention to the signs
Now that you know all about ringworm in cats, it’s your duty to look after the well-being of your small feline. Remember that this disease can be an indication that your cat’s body or environmental conditions aren’t working properly.
Ringworm in cats -also known as dermatophytosis- is a disease in which fungi of various types invade the skin cells, hair, and nails of felines. It’s considered to be the most common fungal infection in cats worldwide. In addition, due to its zoonotic nature, there’s a high risk of transmission from pets to their guardians.
As it’s a major concern for owners, it’s important to know the causes, symptoms, and diagnosis, as well as the best strategies to manage and prevent this important disease in cats. Don’t miss the information below and prepare yourself in the best way in case your feline catches ringworm.
What are the causes of ringworm in cats?
The disease starts with the infection of a cat with fungi called dermatophytes. These microorganisms, having a strong affinity for keratin, attach themselves to the following parts of the host’s body to use them as a source of food and reproduction:
- Skin
- Hair
- Nails
According to an article in the Journal of Feline Medicine and Surgery, the fungus Microsporum canis causes 90% of ringworm in cats, although other types, such as Microsporum gypseum or Trichophyton mentagrophytes, may also be involved.
Transmission can occur by direct contact with an infected feline or with objects contaminated with fungal spores. Among these, the following stand out:
- Nail clippers
- Brushes
- Towels
- Bedding
Although it can occur in cats of any age, breed, or sex, according to the authors of this document, there are certain risk factors for it to occur. Among them, the following can be found:
- Skin lesions: Being the body’s first barrier of defense, a wound in the skin is the ideal entryway for fungi. Attention should be paid to those cats with aggressive play behaviors or that have access to the outdoors. This is because they’re more prone to injury from scratches or bites.
- Immunosuppression: One of the main causes of this condition is prolonged treatment with immunosuppressive drugs such as corticosteroids. Similarly, some studies suggest that cats with diseases such as feline leukemia virus (FLV) and feline immunodeficiency virus (FIV) are more likely to acquire it.
- Ectoparasites: Fleas, in particular, can cause small wounds on the skin. In addition, because of the itching they generate, the cat can hurt itself when scratching.
- Poor hygiene: Inadequate care of the cat can lead to easy colonization by fungi. In addition to this, eradication will be more difficult, as the spores can be spread by the objects used by the pet.
- Overpopulation: In large groups, social stress can predispose cats to suffer from ringworm. In addition, close contact between animals facilitates transmission. Accordingly, stray cats or cats that live in shelters are at high risk of infection.
- Nutritional deficiencies: In particular, diets with low protein and vitamin A levels. These elements play a key role in maintaining a good immune system.
- Young age: Young animals – especially those under one year of age – have an immature immune system. For this reason, their ability to resist infection is more limited. In fact, a study in the Journal of Feline Medicine and Surgery reports that kittens are eight times more likely to suffer ringworm than adults.

What are the symptoms of ringworm infection in cats?
As described above, dermatophytes invade the most keratinous areas of the body, so signs are usually seen in the epidermis, hair follicles, and nails. As stated in an article in The Canadian Veterinary Journal, the following can be distinguished among its symptoms:
- Single or multifocal circular patches with hair loss and desquamation
- Complete areas of alopecia
- Crusty lesions
- Reddening of the skin
- Darkening of the dermis
- Seborrhea
- A strong odor emanating from the cat’s body
- Onychomycosis, which is characterized by weak and brittle nails
- Scratching
As explained in this publication, lesions tend to occur most frequently on the face, ears, and muzzle. However, they can progress to the extremities and other sites, such as the chin.
Can ringworm be transmitted to humans?
The answer to this question is yes. In fact, ringworm is a rapidly spreading pathogen with a high risk of contagion to humans. Moreover, as with pets, young and immunocompromised people are more susceptible to infection by these fungi. This is stated in a paper published in the Journal of Exotic Pet Medicine.
At the same time, a 2022 study reported in the journal Veterinary World reported that people with a history of COVID-19 have a higher risk of suffering from the disease.
Likewise, it’s transmitted through contact with a sick animal or with objects used by the feline. In the event of lesions similar to those described – such as circular patches on the skin – a doctor should be consulted as soon as possible.
How do I know if my cat has ringworm?
Considering that several of these clinical signs are present in other types of skin diseases, the diagnosis should be made by means of laboratory tests. For this, at any sign of disease in your cat, the right thing to do is to see a trained veterinarian immediately.
A paper from the journal Veterinary Dermatology states that different techniques are used to identify the fungus that causes ringworm in cats. The following is a review of some of them.
Wood’s lamp
This is an object that emits and receives ultraviolet light wave radiation. Its efficiency lies in the fact that in the case of dermatophyte infections, such as Microsporum canis, the lamp produces a green luminescence as a result of the chemical interaction of the fungus with a metabolite present in the hair.
Therefore, by bringing it close to the cat’s body at a distance of 1 to 2 inches, the hair follicles acquire a glowy hue.
However, it’s important to note that the absence of this fluorescence doesn’t rule out dermatophyte infection, so other tests must be performed to confirm the diagnosis.
Dermatoscopy and trichography
This consists of observing the condition of the skin and coat of the affected animal in an amplified manner. Thanks to this technique, changes such as darkening of the dermis, desquamation, opaque and slightly curved “comma-shaped” hairs, as well as fungal spores can be seen.
Dermatophyte culture
This is a more accurate method of diagnosis. Once the infected skin or hairs are identified, samples are taken by depilation and are isolated in culture media to observe their growth in the laboratory.
It should be noted that false negatives can be obtained if the sample obtained isn’t from infected hairs. The same is true if the storage and incubation conditions are inadequate or if the culture is contaminated with bacteria or other fungi.
How is ringworm in cats treated?
In the event of a positive result for ringworm, the first step to take is to isolate the infected cat. This will prevent the spread of the fungus to other animals, people, or the environment. Then, depending on the severity of the case, the veterinarian may recommend topical or oral therapy or a combination of both.
In the first case, as described in the article Treatment of dermatophytosis in dogs and cats, cream preparations containing miconazole or ketoconazole and shampoos based on miconazole and 2% chlorhexidine are used.
To avoid infecting a person, these medications should be applied with protective gloves.
At the same time, according to this publication, drugs used for oral or systemic therapy include the following:
- Griseofulvin
- Itraconazole
- Terbinafine
These treatments usually last for long periods of at least one to two months. The reason is that dermatophytes are resistant microorganisms, and if medication is stopped early, they may recur.
Among other things, a study published in the journal BMC Veterinary Research reported the effectiveness of a treatment for cats suffering from ringworm that also had leukemia and feline immunodeficiency virus. In this therapy, a “smart microorganism” was used, called Pythium oligandrum.
Finally, all objects used by the feline should be discarded or disinfected. Among them, the following stand out:
- Brushes
- Scratching posts
- Bedding
- Feeders and drinking bowls
How to prevent ringworm in cats?
As you can see, there are several factors that influence the spread of ringworm in cats. Therefore, these tips will help you prevent this unwanted infection in your pet:
- Offer quality and balanced food to your pet: This is in order to keep its immune system in optimal condition.
- Keep strict control over its deworming and vaccination schedule: This way, you’ll be able to avoid diseases, which are the entryway for dermatophytes.
- Avoid letting your cat outdoors: Being outdoors puts your pet in contact with stray cats that could be contaminated.
- Take adopted cats to a veterinarian: It’s also important to avoid contact with other cats for at least three days.
- Take precautionary measures (use of gloves and isolation): If your cat acquires the fungus, these measures will help prevent contagion.
Pay attention to the signs
Now that you know all about ringworm in cats, it’s your duty to look after the well-being of your small feline. Remember that this disease can be an indication that your cat’s body or environmental conditions aren’t working properly.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Bajwa J. (2020). Feline dermatophytosis: Clinical features and diagnostic testing. The Canadian Veterinary Journal-La revue veterinaire canadienne, 61(11), 1217–1220. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7560770/
- DeTar, L. G., Dubrovsky, V., & Scarlett, J. M. (2019). Descriptive epidemiology and test characteristics of cats diagnosed with Microsporum canis dermatophytosis in a Northwestern US animal shelter. Journal of Feline Medicine and Surgery, 21(12), 1198–1205. https://journals.sagepub.com/doi/10.1177/1098612X19825519?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
- Fehr, M. (2015). Zoonotic Potential of Dermatophytosis in Smalls Mammals. Journal of Exotic Pet Medicine, 24(3), 308-316. https://www.sciencedirect.com/science/article/abs/pii/S1557506315000786
- Frymus, T., Gruffydd-Jones, T., Pennisi, M. G., Addie, D., Belák, S., Boucraut-Baralon, C., Egberink, H., Hartmann, K., Hosie, M. J., Lloret, A., Lutz, H., Marsilio, F., Möstl, K., Radford, A. D., Thiry, E., Truyen, U., & Horzinek, M. C. (2013). Dermatophytosis in cats: ABCD guidelines on prevention and management. Journal of Feline Medicine and Surgery, 15(7), 598–604. https://journals.sagepub.com/doi/10.1177/1098612X13489222
- Jarjees, K. I., & Issa, N. A. (2022). First study on molecular epidemiology of dermatophytosis in cats, dogs, and their companions in the Kurdistan region of Iraq. Veterinary World, 15(12), 2971–2978. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9880842/
- Moriello, K. A., Coyner, K., Paterson, S., & Mignon, B. (2017). Diagnosis and treatment of dermatophytosis in dogs and cats: Clinical Consensus Guidelines of the World Association for Veterinary Dermatology. Veterinary Dermatology, 28(3), 266–e68. https://onlinelibrary.wiley.com/doi/full/10.1111/vde.12440
- Moriello K. A. (2004). Treatment of dermatophytosis in dogs and cats: review of published studies. Veterinary Dermatology, 15(2), 99–107. https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-3164.2004.00361.x?sid=nlm%3Apubmed
- Načeradská, M., Fridrichová, M., Kolářová, M. F., & Krejčová, T. (2021). Novel approach of dermatophytosis eradication in shelters: effect of Pythium oligandrum on Microsporum canis in FIV or FeLV positive cats. BMC Veterinary Research, 17(1), 1-10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8409471/
- Ruiz, A., Medina, D., Maier, L., & Thomson, P. (2019). Dermatofitos en gatos domésticos (Felis catus) positivos a retrovirus. Revista de Investigaciones Veterinarias del Perú, 30(2). http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1609-91172019000200039
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.