Tracheal Collapse in Dogs: Symptoms and Treatment


Written and verified by the vet Daniel Aguilar
We’re sure you know your dog very well and are familiar with their normal behavior. Any changes should be a wake-up call, because it could be the manifestation of a disease. Some respiratory pathologies such as tracheal collapse in dogs need to be diagnosed by professionals, as their symptoms are similar to other problems in the respiratory system.
Not all respiratory signs are caused by pathogens such as viruses and bacteria, as the origin of some pathologies dates back to long ago. From the first moment you see signs of a respiratory condition in your dog, take action. Most of the diseases diagnosed in time have a more favorable prognosis. Read on and find out more about this condition.
What is tracheal collapse?
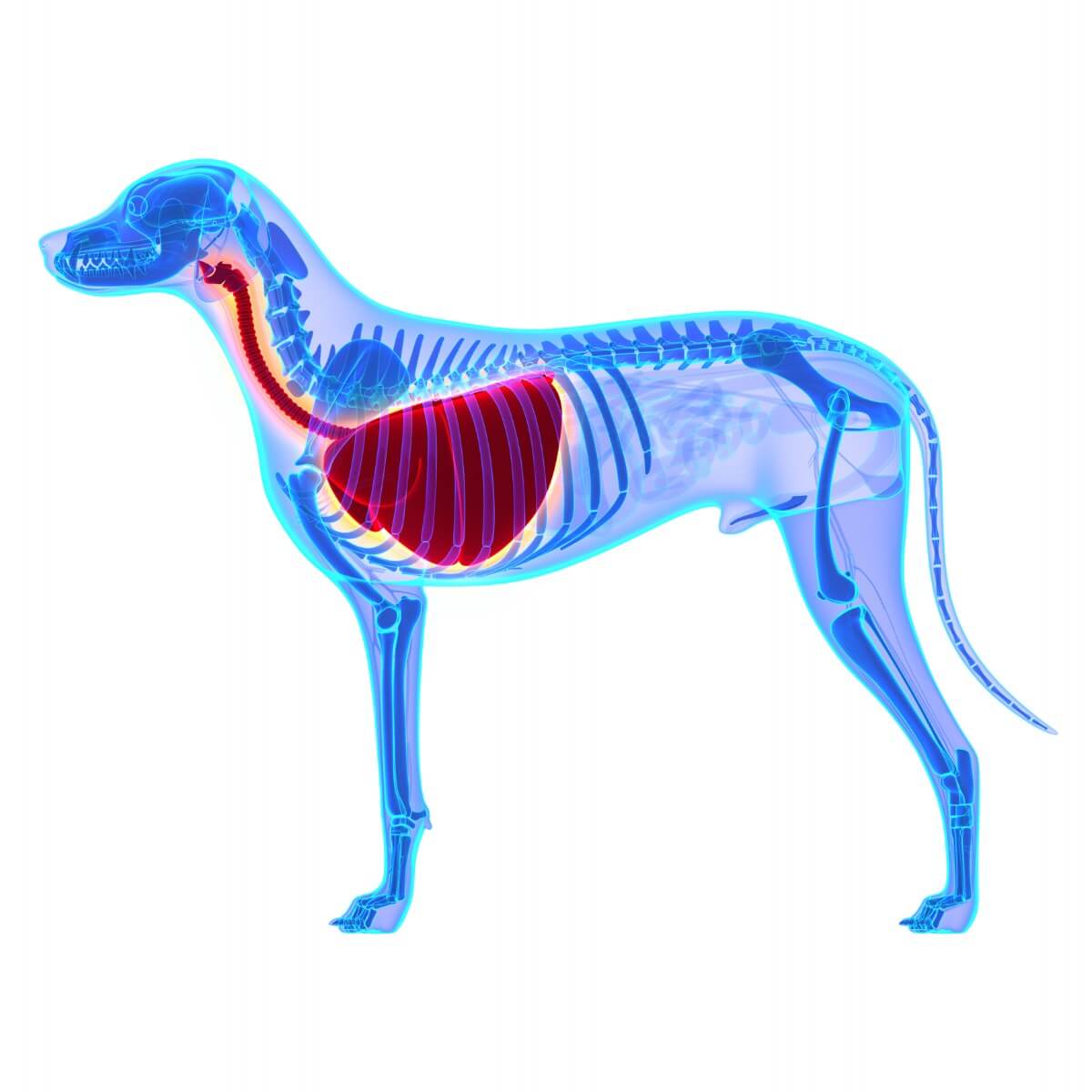
Tracheal collapse in dogs is a disease characterized by a dorsoventral flattening of the trachea. As a result, the lumen of the tracheal tube is reduced and causes severe breathing difficulty in the dog. It’s usually located in the cervical region, although in some dogs it can extend to the bronchi.
Because it’s a disorder of the respiratory tract, it’s common for diseases such as laryngeal and bronchial collapse to occur simultaneously. However, each of the diseases requires individual diagnosis in order to initiate specialized treatment afterward.
The main cause of tracheal collapse in dogs isn’t defined. However, a deficiency of the organic matrix of the tracheal cartilage is considered to play a major role. This deficiency causes the tracheal rings to lack the ability to hold firm and they eventually close.
Taking into account the decrease in the percentage of the lumen in the trachea, tracheal collapse in dogs can be classified into 4 grades:
- I: 25% reduction.
- II: 50% reduction.
- III: 75% reduction.
- IV: A dangerous reduction that sometimes reaches 100%.
Genetic predispositions
Most patients diagnosed with tracheal collapse in dogs are middle-aged and senior dogs. It’s a congenital disease and small breeds such as the Chihuahua, Pomeranian, Poodle, Yorkshire Terrier, Pekingese, and Bichon Maltese are more genetically predisposed to this condition than large breeds.
The average age of onset of symptoms is between 6 and 7 years. Tracheal collapse in dogs is considered a progressive and degenerative pathology. If the signs begin at an early age, the dogs will have less chance of survival.
Symptoms of tracheal collapse in dogs
Respiratory diseases often have very similar signs. In the case of tracheal collapse in dogs, the main sign has been observed to be a characteristic cough, similar to a croak. During times of excitement and physical activity that cause agitation in the canine, the cough usually increases.
If your pet suffers from this disease, it’s likely to also show the following signs:
- Wheezing
- Inspiratory and expiratory dyspnea (shortness of breath)
- Choking
- Nausea
- Abnormal noises perceptible on auscultation
Due to the oxygenation deficit in all organs and systems, the functioning of the canine’s body can be altered and cause secondary pathologies to emerge. Pulmonary hypertension, tracheitis and bronchitis resulting from this collapse are common, and, together, could lead to heart failure.
How is tracheal collapse diagnosed?
To begin with, the veterinarian may ask for an x-ray of the neck and chest. The purpose of this study is to evaluate the structures adjacent to the trachea (heart and lung parenchyma). However, the most useful method to obtain a definitive diagnosis of tracheal collapse in dogs is an endoscopy.
This study allows you to evaluate in detail the progression of the disease and even the degree of severity. Tracheal collapse in dogs is a dynamic pathology, that is to say, it suffers constant changes. Hence the importance of implementing studies such as an endoscopy, which allows you to see in real-time the current status of the problem.
Treatment of tracheal collapse in dogs
Once tracheal collapse in dogs has been diagnosed (along with its degree of progression) it’s time to begin treatment. When the patient is within the first 3 stages of the disease, drugs may be indicated. On the contrary, in dogs that have reached stage 4, surgical intervention will be the only option.
Drugs
In order to reduce the high oxygen demand caused by the excitement and panting, a small dose of tranquilizer is recommended. Subsequently, the veterinarian will decide on the dose of antitussive that’s necessary. Tracheal collapse in dogs usually has a good and rapid response to the use of injectable butorphanol.
As a result of cyanosis, oxygen therapy will be necessary to stabilize the patient. Bronchodilators such as theophylline and some corticosteroids may be prescribed by vets in cases of chronic tracheal collapse. The primary goal of all drugs administered is symptom reduction.
Surgery
As a last resort, if your pet is very severely ill with almost total tracheal lumen obstruction, emergency surgery will be necessary. The veterinarian will perform a rapid evaluation of the patient to qualify them as a candidate for such an intervention. If the patient is suitable, he’ll be taken to the operating room.
There are two options when looking for a solution to tracheal collapse in dogs: reconstruction of the trachea or placement of an endoprosthesis (provides artificial support for the trachea and prevents it from closing). Both procedures require certain post-operative care, as well as close monitoring by your veterinarian.

As you may have noticed, tracheal collapse in dogs can be a very dangerous (even lethal) condition. If you have a pet at home with the characteristics mentioned above, the best way to avoid complications and secondary conditions is to report any abnormalities in a timely manner. The health of your best friend is in your hands.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- Castellanos L. Colapso traqueal en el perro. México. Publicado en julio de 1991. Consultado el 07 de octubre de 2021. Disponible en: https://repositorio.unam.mx/contenidos/colapso-traqueal-en-el-perro-3430965?c=3AQXbo&d=false&q=*:*&i=8&v=1&t=search_0&as=0
- Rueda J. Colapso traqueal. Madrid, España. Publicado en 1989. Consultado el 07 de octubre de 2021. Disponible en: https://ddd.uab.cat/pub/clivetpeqani/11307064v9n4/11307064v9n4p165.pdf
- Coello Z. Colapso traqueal en perros – Síntomas y tratamiento. España. Publicado el 13 de diciembre de 2016. Consultado el 07 de octubre de 2021. Disponible en: https://www.expertoanimal.com/colapso-traqueal-en-perros-sintomas-y-tratamiento-22336.html
- Colapso traqueal. Ciudad de México. Consultado el 07 de octubre de 2021. Disponible en: https://hospitalveterinariodelta.com.mx/especialidades/cirugia-de-tejidos-blandos/colapso-traqueal/
- Romairone A. Colaptos traqueal en perro. Argentina. Publicado el 20 de mayo de 2015. Consultado el 07 de octubre de 2021. Disponible en: https://www.diagnosticoveterinario.com/colapso-traqueal-en-perro/3887
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.