Antibiotic Resistance in Pets: Why Is It a Threat?


Written and verified by the veterinarian and zootechnician Sebastian Ramirez Ocampo
Thanks to advances in the field of veterinary medicine, animal welfare has achieved developments that could never have been imagined. However, threats such as antibiotic resistance in pets may jeopardize some of what has been achieved so far. This is due to the transmission of superbugs from dogs and cats to their owners.
Although the increased survival capacity of microorganisms against drugs that previously affected them is a problem that affects humans to a greater extent, several studies have warned about the implications of this phenomenon in pets.
If you want to learn more about the causes, implications and risks of antibiotic resistance in pets, don’t miss the information we’ll share with you in this article.
The use of antibiotics in veterinary medicine
Since their discovery in 1928 by physician Alexander Fleming, antibiotics have saved the lives of millions of people around the world. For the first time, a drug was able to effectively fight bacteria and microbes that caused diseases of different kinds.
In the field of veterinary medicine, antibiotics were introduced about 70 years ago. Since then, thanks to these compounds, the life expectancy of pets has been prolonged.
Because of their bacteriostatic and bactericidal action, i.e. they kill microorganisms and also prevent their multiplication, these drugs have been successfully used in the treatment of ocular, dermal, ear, respiratory and urinary pathologies.
However, bacteria have managed to circumvent the effects of antimicrobial agents. They have developed genetic mutations that allow them to resist the actions of these chemicals on their cellular integrity.

What is antibiotic resistance and how is it generated?
In clinical terms, this phenomenon is defined as the ability of a bacterium to resist the effects of a drug that previously affected it. In essence, microorganisms evolve to a point where they can survive and reproduce despite exposure to an antibiotic to which they were previously sensitive.
This ability is generated by genetic changes or mutations in the bacteria’s DNA, which can be transferred to subsequent generations or to other bacteria of different species.
Although not all the elements involved in antibiotic resistance have been clearly established, certain risk factors for its occurrence have been identified.
- Overexposure to antibiotics: No matter how effective a drug is, it can rarely if ever kill 100% of a bacterial colony. For this reason, there’ll be at least one microorganism that has survived its effect. The risk is that it will pass on its genetic material to its offspring, thus creating new microorganisms resistant to that antibiotic.
- Giving antimicrobial agents at ineffective doses: In veterinary practice, it’s common that, due to a lack of knowledge, antibiotics are prescribed at inadequate doses. That is, below the threshold of effectiveness. This situation generates a higher bacterial survival rate, which will also acquire a progressive resistance to the drug.
- Use broad-spectrum antibiotics: Although these types of drugs act effectively against a wide range of bacteria, their overuse can lead to antibiotic resistance by different infectious agents.
Antibiotic resistance in pets
Several studies have identified resistant strains of bacteria in companion animals such as dogs and cats. The data from these investigations have made it possible to determine the variables associated with this problem.
For example, a study shared in the journal Veterinary Microbiology detailed the presence of bacteria of the species Staphylococcus intermedius resistant to penicillins, macrolides, tetracyclines, and chloramphenicol in dogs with pyoderma.
Similarly, a paper in the Journal of the American Veterinary Medical Association reported the finding of Escherichia coli resistant to fluoroquinolones in dogs with urinary tract infections.
In addition, an investigation conducted in Colombia found Staphylococcus spp resistant to ampicillin, cephalosporin, enrofloxacin and tetracycline in dogs and cats. Other infectious agents such as Klebsiella spp, Enterococcus spp, Pseudomonas aeruginosa and Staphylococcus aureus have also been identified.
Risk factors for acquiring resistant bacterial infections in pets include the following:
- Prolonged hospitalization times: This creates greater exposure to these agents.
- Immunosuppressive diseases: Pathologies such as feline immunodeficiency virus produce a greater susceptibility to acquiring this type of bacteria.
- Sick animals: Transmission of resistant microorganisms can occur through contact with infected pets.
- Raw meat-based foods, also known as BARF diets, make pets more likely to carry bacteria resistant to these drugs.
Implications of this problem
Antibiotic resistance is a challenge for human and animal health professionals, because it creates many problems for both pets and those responsible for them.
On the one hand, treatment of this type of bacteria is more expensive. This is due to the fact that the drugs needed are usually more expensive than those used in conventional situations.
In addition to this, patients need more visits to the veterinarian, since a strict control of their evolution must be carried out. In addition, diagnostic tests are necessary to evaluate the pharmacological sensitivity of the microorganisms.
On the other hand, pets under these treatments usually show more adverse effects due to the potency of the drugs used. As an example, a study published in the journal Veterinary Dermatology, which evaluated the treatment of 216 dogs with pyoderma, reported greater adverse reactions at the gastrointestinal level in dogs under therapy against resistant bacteria.
The risk of antibiotic resistance in pets for those responsible for their care
According to an article published in the journal Microorganisms, these microorganisms have the ability to spread through human-animal contact, creating what are known as zoonotic diseases.
In addition, genes that play a key role in bacterial resistance can be transmitted between humans and pets. For example, research published in the Journal of Applied Microbiology identified – by PCR – genes involved in bacterial resistance in stool samples from dogs and owners.
Of these, an average of 3.3 were shared between humans and their pets. Although the proportion is low, the authors indicate that resistant bacteria in companion animals should be continuously analyzed. This is because of the risk that this situation represents for public health.
What to do in the face of this situation?
It is estimated that about 50% of antibiotics prescribed in humans are prescribed unnecessarily or improperly managed. In the area of veterinary medicine, it’s believed that something similar occurs. Accordingly, healthcare professionals must be the first to take responsibility and take action to curb the advance of resistant and multidrug-resistant bacteria.
As the rate at which new antibiotics are being discovered has slowed considerably, veterinarians must be increasingly selective in their use of these drugs in their patients.

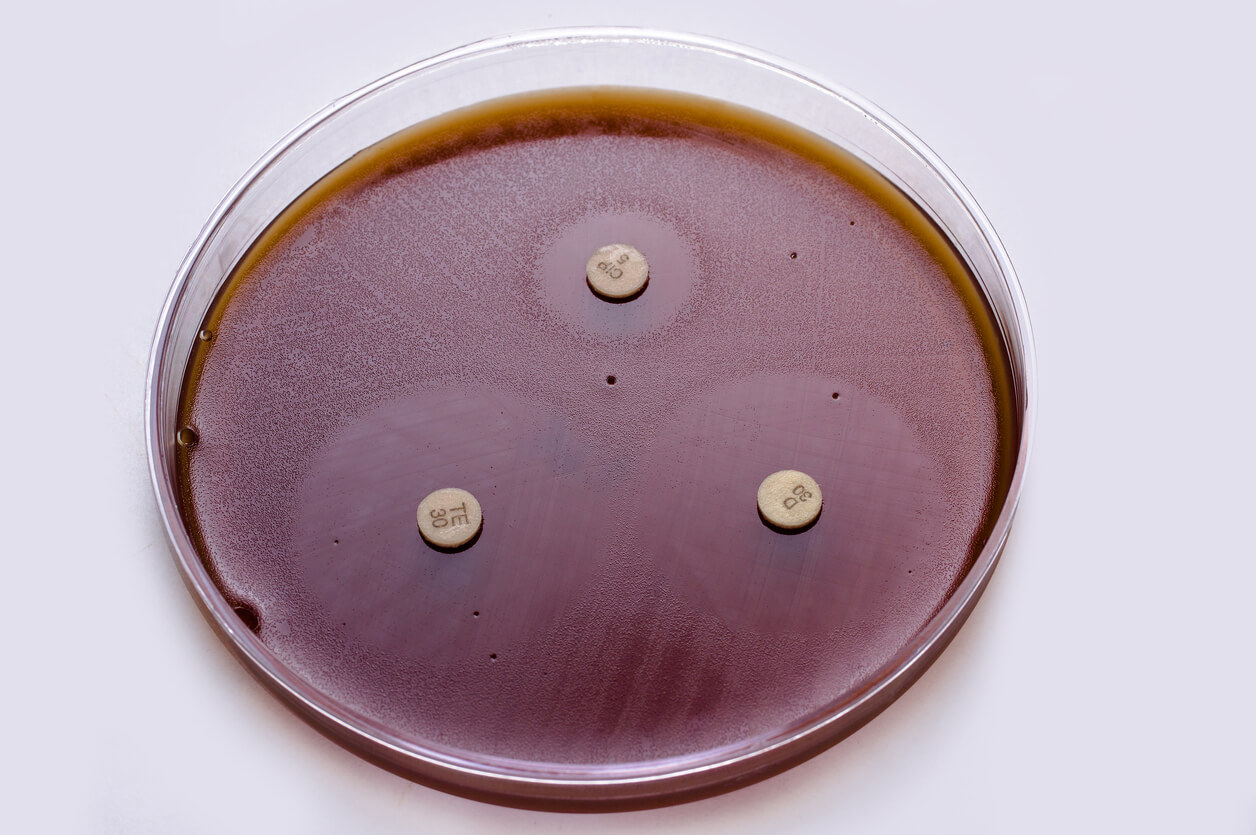
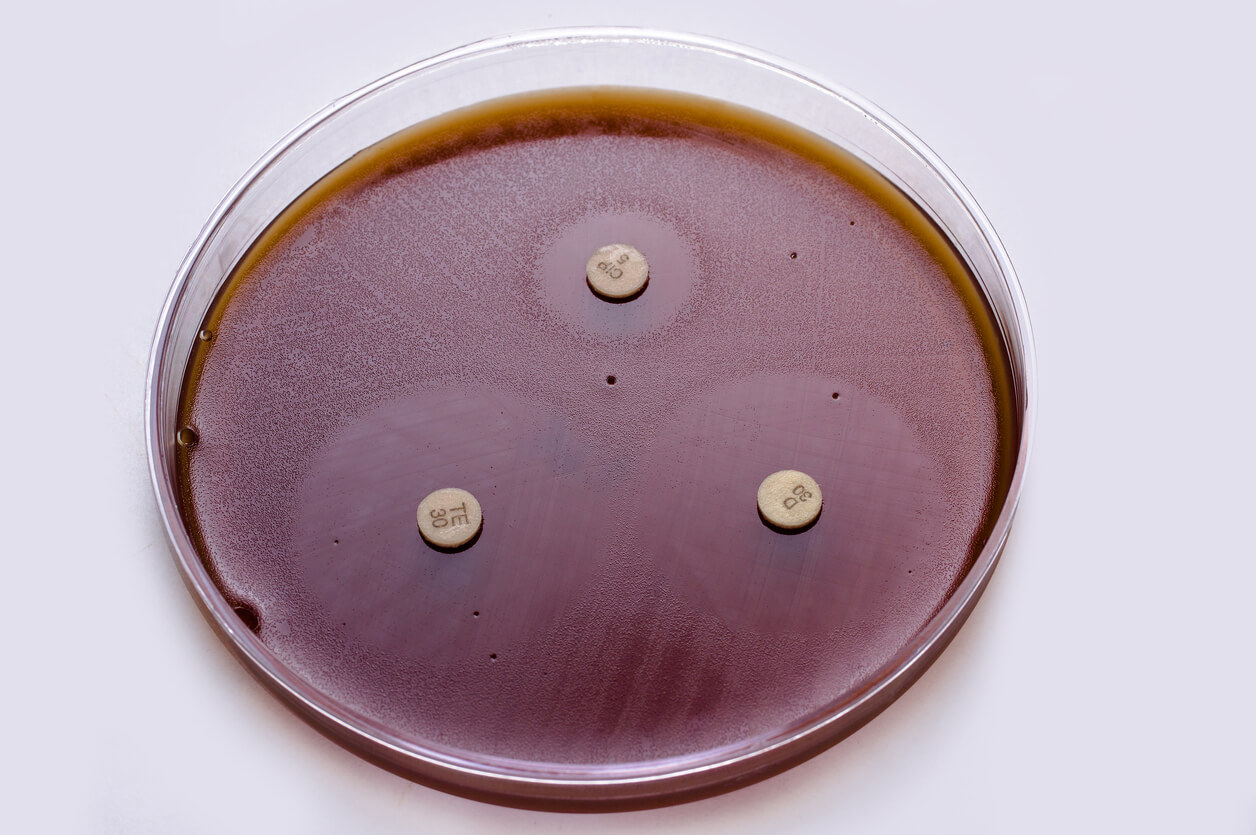
Developing strategies such as the routine use of antibiograms to detect the sensitivity of a bacterium or ensuring that the correct doses are administered at the right frequency and time should be the mission of each of the professionals involved.
In fact, the American Veterinary Medical Association (AVMA) has developed a series of practical tools that allow veterinarians to make evidence-based decisions when treating their patients.
Finally, veterinarians should avoid practices such as empirical medication of their pets. In addition to keeping the vaccination and deworming schedules of their dogs or cats up to date. Finally, it’s important to remember the need for constant check-ups, as it’s always better to be safe than sorry.
Thanks to advances in the field of veterinary medicine, animal welfare has achieved developments that could never have been imagined. However, threats such as antibiotic resistance in pets may jeopardize some of what has been achieved so far. This is due to the transmission of superbugs from dogs and cats to their owners.
Although the increased survival capacity of microorganisms against drugs that previously affected them is a problem that affects humans to a greater extent, several studies have warned about the implications of this phenomenon in pets.
If you want to learn more about the causes, implications and risks of antibiotic resistance in pets, don’t miss the information we’ll share with you in this article.
The use of antibiotics in veterinary medicine
Since their discovery in 1928 by physician Alexander Fleming, antibiotics have saved the lives of millions of people around the world. For the first time, a drug was able to effectively fight bacteria and microbes that caused diseases of different kinds.
In the field of veterinary medicine, antibiotics were introduced about 70 years ago. Since then, thanks to these compounds, the life expectancy of pets has been prolonged.
Because of their bacteriostatic and bactericidal action, i.e. they kill microorganisms and also prevent their multiplication, these drugs have been successfully used in the treatment of ocular, dermal, ear, respiratory and urinary pathologies.
However, bacteria have managed to circumvent the effects of antimicrobial agents. They have developed genetic mutations that allow them to resist the actions of these chemicals on their cellular integrity.

What is antibiotic resistance and how is it generated?
In clinical terms, this phenomenon is defined as the ability of a bacterium to resist the effects of a drug that previously affected it. In essence, microorganisms evolve to a point where they can survive and reproduce despite exposure to an antibiotic to which they were previously sensitive.
This ability is generated by genetic changes or mutations in the bacteria’s DNA, which can be transferred to subsequent generations or to other bacteria of different species.
Although not all the elements involved in antibiotic resistance have been clearly established, certain risk factors for its occurrence have been identified.
- Overexposure to antibiotics: No matter how effective a drug is, it can rarely if ever kill 100% of a bacterial colony. For this reason, there’ll be at least one microorganism that has survived its effect. The risk is that it will pass on its genetic material to its offspring, thus creating new microorganisms resistant to that antibiotic.
- Giving antimicrobial agents at ineffective doses: In veterinary practice, it’s common that, due to a lack of knowledge, antibiotics are prescribed at inadequate doses. That is, below the threshold of effectiveness. This situation generates a higher bacterial survival rate, which will also acquire a progressive resistance to the drug.
- Use broad-spectrum antibiotics: Although these types of drugs act effectively against a wide range of bacteria, their overuse can lead to antibiotic resistance by different infectious agents.
Antibiotic resistance in pets
Several studies have identified resistant strains of bacteria in companion animals such as dogs and cats. The data from these investigations have made it possible to determine the variables associated with this problem.
For example, a study shared in the journal Veterinary Microbiology detailed the presence of bacteria of the species Staphylococcus intermedius resistant to penicillins, macrolides, tetracyclines, and chloramphenicol in dogs with pyoderma.
Similarly, a paper in the Journal of the American Veterinary Medical Association reported the finding of Escherichia coli resistant to fluoroquinolones in dogs with urinary tract infections.
In addition, an investigation conducted in Colombia found Staphylococcus spp resistant to ampicillin, cephalosporin, enrofloxacin and tetracycline in dogs and cats. Other infectious agents such as Klebsiella spp, Enterococcus spp, Pseudomonas aeruginosa and Staphylococcus aureus have also been identified.
Risk factors for acquiring resistant bacterial infections in pets include the following:
- Prolonged hospitalization times: This creates greater exposure to these agents.
- Immunosuppressive diseases: Pathologies such as feline immunodeficiency virus produce a greater susceptibility to acquiring this type of bacteria.
- Sick animals: Transmission of resistant microorganisms can occur through contact with infected pets.
- Raw meat-based foods, also known as BARF diets, make pets more likely to carry bacteria resistant to these drugs.
Implications of this problem
Antibiotic resistance is a challenge for human and animal health professionals, because it creates many problems for both pets and those responsible for them.
On the one hand, treatment of this type of bacteria is more expensive. This is due to the fact that the drugs needed are usually more expensive than those used in conventional situations.
In addition to this, patients need more visits to the veterinarian, since a strict control of their evolution must be carried out. In addition, diagnostic tests are necessary to evaluate the pharmacological sensitivity of the microorganisms.
On the other hand, pets under these treatments usually show more adverse effects due to the potency of the drugs used. As an example, a study published in the journal Veterinary Dermatology, which evaluated the treatment of 216 dogs with pyoderma, reported greater adverse reactions at the gastrointestinal level in dogs under therapy against resistant bacteria.
The risk of antibiotic resistance in pets for those responsible for their care
According to an article published in the journal Microorganisms, these microorganisms have the ability to spread through human-animal contact, creating what are known as zoonotic diseases.
In addition, genes that play a key role in bacterial resistance can be transmitted between humans and pets. For example, research published in the Journal of Applied Microbiology identified – by PCR – genes involved in bacterial resistance in stool samples from dogs and owners.
Of these, an average of 3.3 were shared between humans and their pets. Although the proportion is low, the authors indicate that resistant bacteria in companion animals should be continuously analyzed. This is because of the risk that this situation represents for public health.
What to do in the face of this situation?
It is estimated that about 50% of antibiotics prescribed in humans are prescribed unnecessarily or improperly managed. In the area of veterinary medicine, it’s believed that something similar occurs. Accordingly, healthcare professionals must be the first to take responsibility and take action to curb the advance of resistant and multidrug-resistant bacteria.
As the rate at which new antibiotics are being discovered has slowed considerably, veterinarians must be increasingly selective in their use of these drugs in their patients.

Developing strategies such as the routine use of antibiograms to detect the sensitivity of a bacterium or ensuring that the correct doses are administered at the right frequency and time should be the mission of each of the professionals involved.
In fact, the American Veterinary Medical Association (AVMA) has developed a series of practical tools that allow veterinarians to make evidence-based decisions when treating their patients.
Finally, veterinarians should avoid practices such as empirical medication of their pets. In addition to keeping the vaccination and deworming schedules of their dogs or cats up to date. Finally, it’s important to remember the need for constant check-ups, as it’s always better to be safe than sorry.
All cited sources were thoroughly reviewed by our team to ensure their quality, reliability, currency, and validity. The bibliography of this article was considered reliable and of academic or scientific accuracy.
- American Veterinary Medical Association. Antimicrobial use and antimicrobial resistance pet owner FAQ. Consultado el 10 de mayo de 2023. https://www.avma.org/resources-tools/one-health/antimicrobial-use-and-antimicrobial-resistance/antimicrobial-use-and-antimicrobial-resistance-pet-owner-faq
- American Veterinary Medical Association. Antimicrobial use and antimicrobial resistance. Consultado el 5 de mayo de 2023. https://www.avma.org/resources-tools/one-health/antimicrobial-use-and-antimicrobial-resistance
- American Veterinary Medical Association. Antimicrobial use in veterinary practice. Consultado el 8 de mayo de 2023. https://www.avma.org/resources-tools/one-health/antimicrobial-use-and-antimicrobial-resistance/antimicrobial-use-veterinary-practice
- Bryan, J., Frank, L. A., Rohrbach, B. W., Burgette, L. J., Cain, C. L., & Bemis, D. A. (2012). Treatment outcome of dogs with meticillin-resistant and meticillin-susceptible Staphylococcus pseudintermedius pyoderma. Veterinary Dermatology, 23(4), 361–e65. https://onlinelibrary.wiley.com/doi/10.1111/j.1365-3164.2012.01034.x
- Frey E. (2018). The role of companion animal veterinarians in one-health efforts to combat antimicrobial resistance. Journal of the American Veterinary Medical Association, 253(11), 1396–1404. https://avmajournals.avma.org/view/journals/javma/253/11/javma.253.11.1396.xml#ref8
- Gómez-Beltrán, D. A., Villar, D., López-Osorio, S., Ferguson, D., Monsalve, L. K., & Chaparro-Gutiérrez, J. J. (2020). Prevalence of Antimicrobial Resistance in Bacterial Isolates from Dogs and Cats in a Veterinary Diagnostic Laboratory in Colombia from 2016–2019. Veterinary Sciences, 7(4), 173. https://www.mdpi.com/2306-7381/7/4/173
- Guardabassi, L., Loeber, M. E., & Jacobson, A. (2004). Transmission of multiple antimicrobial-resistant Staphylococcus intermedius between dogs affected by deep pyoderma and their owners. Veterinary Microbiology, 98(1), 23–27. https://www.sciencedirect.com/science/article/abs/pii/S0378113503003584?via%3Dihub
- Hardefeldt, L. Y., Hur, B., Richards, S., Scarborough, R., Browning, G. F., Billman-Jacobe, H., Gilkerson, J. R., Ierardo, J., Awad, M., Chay, R., & Bailey, K. E. (2022). Antimicrobial stewardship in companion animal practice: an implementation trial in 135 general practice veterinary clinics. JAC-Antimicrobial Resistance, 4(1), dlac015. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8874133/
- Ogeer-Gyles, J., Mathews, K., Weese, J. S., Prescott, J. F., & Boerlin, P. (2006). Evaluation of catheter-associated urinary tract infections and multi-drug-resistant Escherichia coli isolates from the urine of dogs with indwelling urinary catheters. Journal of the American Veterinary Medical Association, 229(10), 1584–1590. https://avmajournals.avma.org/view/journals/javma/229/10/javma.229.10.1584.xml
- Rahman, M. T., Sobur, M. A., Islam, M. S., Ievy, S., Hossain, M. J., El Zowalaty, M. E., … & Ashour, H. M. (2020). Zoonotic diseases: etiology, impact, and control. Microorganisms, 8(9), 1405. https://www.mdpi.com/2076-2607/8/9/1405
- Rumi, M. V., Nuske, E., Mas, J., Argüello, A., Gutkind, G., & Di Conza, J. (2021). Antimicrobial resistance in bacterial isolates from companion animals in Buenos Aires, Argentina: 2011-2017 retrospective study. Zoonoses and public health, 68(5), 516–526. https://onlinelibrary.wiley.com/doi/10.1111/zph.12842
- Røken, M., Forfang, K., Wasteson, Y., Haaland, A. H., Eiken, H. G., Hagen, S. B., & Bjelland, A. M. (2022). Antimicrobial resistance-Do we share more than companionship with our dogs?. Journal of Applied Microbiology, 133(2), 1027–1039. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9542740/
- Umber, J. K., & Bender, J. B. (2009). Pets and antimicrobial resistance. The Veterinary clinics of North America. Small animal practice, 39(2), 279–292. https://www.sciencedirect.com/science/article/abs/pii/S0195561608001939?via%3Dihub
- White, D., McDermott (2001). Emergence and Transfer of Antibacterial Resistance. Journal of Dairy Science, 84, e151-e155. https://www.sciencedirect.com/science/article/pii/S0022030201702093
- Yang, Y., Hu, X., Li, W., Li, L., Liao, X., & Xing, S. (2022). Abundance, diversity and diffusion of antibiotic resistance genes in cat feces and dog feces. Environmental pollution (Barking, Essex : 1987), 292(Pt A), 118364. https://linkinghub.elsevier.com/retrieve/pii/S0269-7491(21)01946-1
This text is provided for informational purposes only and does not replace consultation with a professional. If in doubt, consult your specialist.